mental health
mental health
Evidence, Biology, and Evolving Perspectives
Mental health is one of the most complex and debated areas of modern medicine. Definitions, diagnoses, and treatments have shifted significantly over time, often reflecting changes in scientific understanding as well as cultural interpretation. Clinicians define most mental health disorders by reported symptoms rather than objective laboratory tests. Therefore, serious examination requires both scientific rigor and historical awareness. Our goal is not to repeat prevailing narratives but to evaluate mental health through biological, social, philosophical, and long-term outcome frameworks.
Despite decades of neuroscience research, the brain remains only partially understood. Neurotransmitter systems such as serotonin and dopamine are frequently cited in psychiatric treatment models; however, receptor interactions, network signaling, and long-term neuroadaptation are far more complex than simplified explanations suggest. Notably, a substantial portion of serotonin receptors are located in the gastrointestinal tract, underscoring the interconnected nature of the gut–brain axis. Consequently, emerging research in metabolic psychiatry, inflammation, and nutritional neuroscience has expanded discussion beyond narrow chemical imbalance models. While traditional pharmacology remains influential, newer lines of inquiry suggest that mental health may involve systemic processes extending beyond isolated neurotransmitter levels.
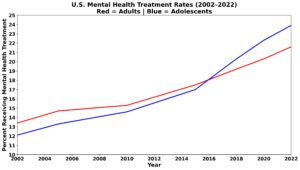
Over the past several decades, psychotropic medication use has increased substantially in the United States. National surveys and prescription databases commonly estimate that clinicians prescribe antidepressants, stimulants, antipsychotics, or mood stabilizers to approximately 50 to 60 million Americans each year. That figure represents roughly one in five adults. During the same period, reported rates of depression, anxiety, and suicide have not uniformly declined and in some populations have increased. Although correlation does not prove causation, these parallel trends raise important questions about long-term effectiveness and treatment durability.
Mental health spending reflects the scale of this issue. National health expenditure data show that Americans spend tens of billions of dollars annually on psychotropic medications. Depending on the year and drug class included, prescription antidepressant spending alone has reached into the multi-billion-dollar range annually. When broader categories such as antipsychotics and ADHD medications are included, total psychiatric drug expenditures expand significantly. These figures do not in themselves imply misconduct; however, they illustrate the magnitude of reliance on pharmaceutical approaches within modern mental health care. Therefore, examining long-term outcomes and cost–benefit profiles becomes increasingly important.
Our methodology prioritizes long-term evidence over short-term symptom change. Many psychiatric clinical trials measure outcomes over six to eight weeks, whereas mental health conditions often persist for years or decades. Accordingly, we evaluate durability of benefit, relapse rates, functional recovery, and quality-of-life outcomes in addition to short-term symptom scales. When evidence is limited or contested, we clearly state those limitations. In addition to peer-reviewed scientific papers, we examine foundational books in psychiatry, psychology, neuroscience, and philosophy. We also review long-form interviews and expert discussions; however, we evaluate all claims against available research and methodological standards.
Mental health does not exist in isolation from social structure. Family systems, community cohesion, trauma exposure, economic instability, nutrition, and cultural expectations all influence psychological well-being. Furthermore, research increasingly explores the role of spirituality, religious participation, and belief systems in resilience and coping. While spirituality cannot be reduced to a clinical intervention, its relationship to meaning-making and social integration warrants thoughtful, research-based examination.
Mental health does not exist in isolation from social structure. Family systems, community cohesion, trauma exposure, economic instability, nutrition, and cultural expectations all influence psychological well-being. Furthermore, research increasingly explores the role of spirituality, religious participation, and belief systems in resilience and coping. While spirituality cannot be reduced to a clinical intervention, its relationship to meaning-making and social integration warrants thoughtful, research-based examination.
What is mental health?
Mental health definitions have evolved significantly across decades, reflecting shifts in medical theory, cultural norms, and clinical practice. This pillar examines how diagnostic frameworks developed, including the expansion of criteria in successive editions of major psychiatric manuals. By tracing these changes, we aim to distinguish enduring scientific findings from evolving classification systems.
Understanding diagnosis requires careful examination of how disorders are defined and measured. Unlike many physical conditions, mental health diagnoses often rely on symptom clusters and behavioral observations rather than biological tests. Therefore, this section evaluates how diagnostic thresholds are set, how categories are debated, and how cultural context can influence interpretation.
Finally, this topic explores the historical roots of mental health treatment, from early institutional care to modern outpatient models. By examining past approaches and paradigm shifts, we provide perspective on how current frameworks emerged. This historical grounding supports thoughtful analysis rather than reactive acceptance or rejection of prevailing narratives.
Brain Biology, Neurotransmitters & the Gut–Brain Axis
Here we examine the biological foundations of mental health, including neurotransmitter systems, receptor complexity, neural circuitry, inflammation, and the gut–brain connection. Rather than relying on simplified chemical imbalance narratives, we explore emerging research in metabolic psychiatry, neuroplasticity, and systemic regulation. The goal is to clarify what neuroscience currently supports and where meaningful uncertainty remains.
mental health in Spirituality, Meaning & Human Suffering
Here we investigate the role of meaning, belief systems, and spiritual formation in psychological resilience. Research increasingly suggests that purpose, community participation, and existential coherence influence mental health outcomes. Rather than reducing spirituality to a clinical intervention, this section evaluates its potential contribution to coping, recovery, and long-term well-being within a research-based framework.
Social Structure, Family Systems & Cultural Influences
Mental health does not develop in isolation from social context. We explore the role of family cohesion, community stability, trauma exposure, economic stress, and institutional shifts in shaping psychological well-being. By examining research on loneliness, homelessness, and social fragmentation, we broaden understanding beyond purely biological explanations.
Psychiatric Treatment: Evidence, Duration & Long-Term Outcomes
This section evaluates psychiatric treatment models through the lens of long-term evidence. We examine clinical trial duration, relapse rates, comparative effectiveness, and risk–benefit profiles while distinguishing short-term symptom change from durable recovery. By focusing on methodological rigor and outcome sustainability, this pillar seeks to move beyond surface-level efficacy claims.